Every baby has their own nutritional needs and going home might bring up questions for you on how to support them best.
Breastfeeding offers many benefits for both you and your baby, including important skin-to-skin contact that helps you bond. However, some babies, especially those born preterm or unwell, may not be ready or able to breastfeed for long enough to get what they need. It is quite normal for parents, even experienced ones, that time is needed to gain confidence in breastfeeding, especially when their baby is preterm or sick.
You might hear unhelpful comparisons from others, but what matters is your baby’s individual progress. Having support can make a big difference and you can always ask for advice from your healthcare team at the hospital before discharge. If your baby is born very early, try to connect with other parents who have experience with preterm babies.
Before you start breastfeeding at home, you will get support from the neonatal unit staff, or you can contact your local breastfeeding support service. They can help you find a suitable breast pump and teach you how to express your milk by hand.
Feeding a preterm baby can come with unique challenges, but there are several options to make sure that your baby gets the nutrition they need to grow and thrive. Whether you fully breastfeed, bottle feed, combine breast milk with fortifiers⍰, or use formula⍰ your healthcare team will be there to support you and answer any questions you may have.
By the time your baby is ready to go home, their doctor or dietitian⍰ will tell you if you still need to use fortifiers after leaving the hospital.
Preterm babies often benefit from expressed breast milk with added fortifiers because sometimes their small bodies require more concentrated nutrition than breast milk or regular formula alone can provide. These fortifiers come in powder form, made from donor human milk or processed cow's milk with added nutrients.
Breast milk is the best option for your baby, but sometimes breastfeeding is not possible for various reasons. In these cases, feeding your baby formula will meet your baby’s specific nutritional needs. For some preterm babies a formula with extra iron, fat, protein, calcium, and other important vitamins and minerals is advised to help them grow adequately. More specialized formulas may be needed in certain situations, such as if your baby has had surgery. Your healthcare team will recommend the best formula for your baby and can help to make sure you have ongoing access to it after discharge as some formula milks may need to be prescribed.
Some parents choose combination feeding, which involves offering both breast milk and formula. This approach can give your baby the benefits of breast milk while ensuring they get the extra nutrition they need from formula. Your healthcare team can support you in finding the best feeding plan for you and your baby.
If you choose to bottle feed, your baby's healthcare team will guide you once your baby is ready to try it for the first time. Like breastfeeding, preterm babies need time to grow, mature, and learn how to suck, swallow, and breathe at the same time. Keep in mind that preterm babies might get tired or sleepy during feedings and may need more time and patience. It will get easier for both you and your baby over time.
Read more about bottle feeding.
To learn about alternative feeding methods, ask your midwife⍰ or a lactation consultant⍰.
The process of introducing a baby to solid foods is known as complementary feeding. If your baby was born at term but sick, you might also find the information in this section helpful. Always consult with your healthcare professional for personalized advice, as your baby's care will depend on specific conditions and their current health status.
In this context, weaning means gradually introducing your baby to solid foods while they continue to have milk. It does not mean suddenly stopping milk feeds, but rather adding solids alongside milk as your baby grows.
Parents might worry about how their baby will handle weaning after a challenging start in life, especially parents of preterm babies often find it hard to know when to begin weaning. This is because preterm babies may develop more slowly than full-term babies, so they might for example sit up later. The recommendations below will help you know when your baby may be ready to start weaning, taking their development into account.
Tips for successful weaning
All babies reach a point where they are ready to try solid foods along with their milk. Your baby will slowly learn how to hold and explore the food they are given by touching, tasting, and smelling it. As time goes on, you will notice that your baby will need less help to sit up and will start bringing food and toys to their mouth on their own. They will push food out with their tongue less often and learn to bite and chew. With practice, they will also learn to drink from a cup, beaker, or straw.
Your baby will pick up eating skills by watching you eat. Mealtimes are a great opportunity for this because they are fun and social. Eating together as a family helps both, you and your baby learn about weaning. Follow your baby’s pace and do not worry if progress seems to be slow. Stay with your baby during meals, encourage them to touch and explore food, and stop offering food if they show signs of disinterest or lack of hunger. Forcing your baby to eat can cause distress and food refusal.
You may be thinking about adding solids to your baby’s bottle or feeding pureed food from a pouch to make the transition easier. However, this is not recommended and does not help them learn essential eating skills. If you have concerns about your baby’s weaning progress, discuss them with your healthcare provider.
Signs your baby is ready for weaning
Look for these signs that your baby is ready to start weaning:
It is important not to mistake other behaviors for readiness to wean. Increased milk consumption might indicate a growth spurt rather than a need for solids. Waking up more at night can also be due to growth or developmental changes. There is no specific weight your baby needs to reach to start weaning, and the presence of teeth does not necessarily mean they are ready for solid food.
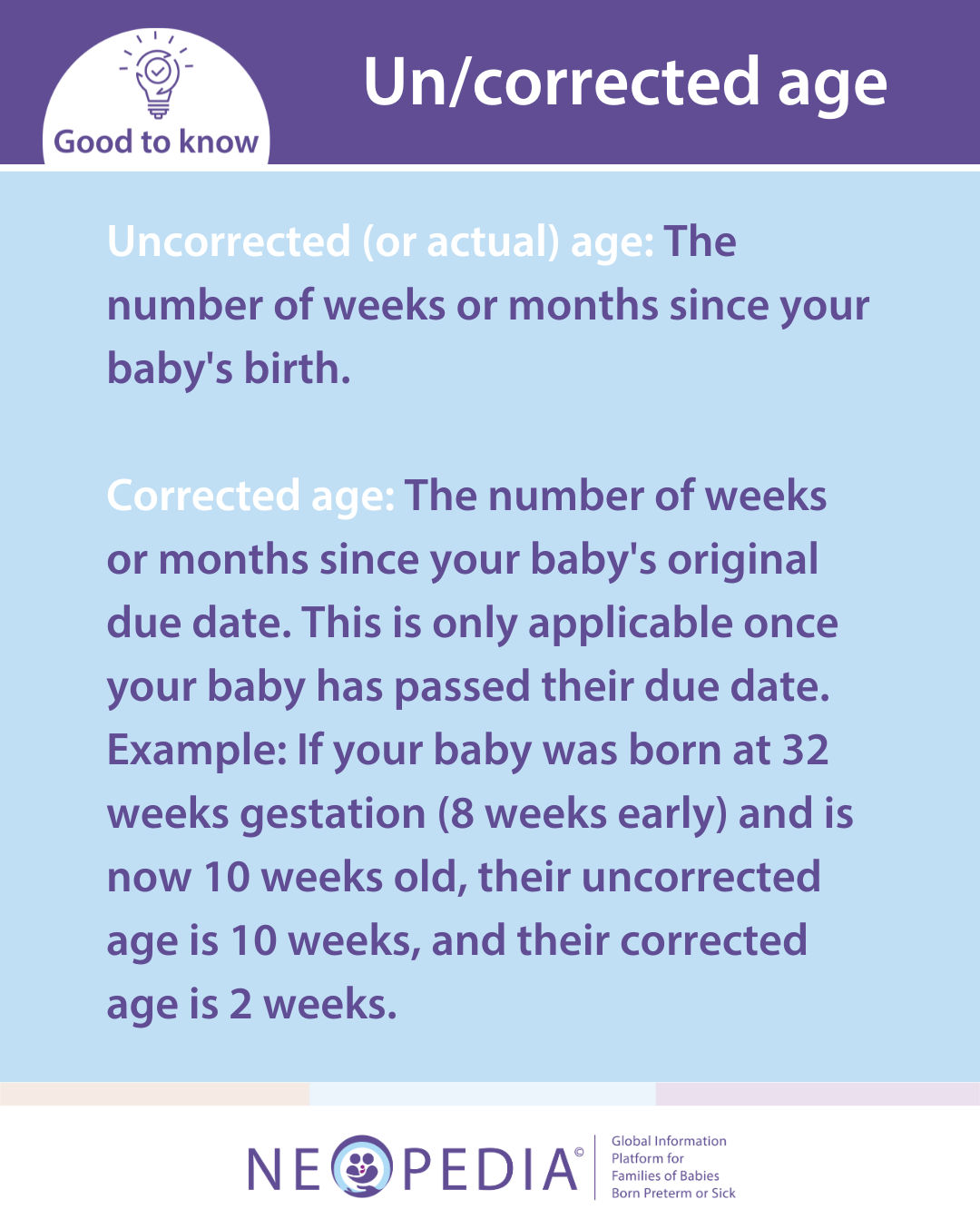
Read more about “corrected age” and “uncorrected age”.
Recommended weaning timeline for preterm babies
Start weaning when your baby shows feeding signs, usually around six months corrected age, but avoid starting before five months corrected age. Aim to introduce mashed or softly textured foods by about seven months corrected age. If your baby is not showing signs of being ready for solid foods by seven months corrected age, be patient and seek a second opinion from your healthcare provider.
Which foods to choose for weaning?
There are no special first foods that are better for preterm babies.
If you are considering a vegetarian or vegan diet for your baby, seek advice from your healthcare provider. Avoid salty or sugary foods, and do not add salt, sugar, or honey to your baby’s meals. Be aware that this also means to avoid adding salt to any cooking water.
Some initial foods to consider include:
As your baby progresses with weaning try these finger foods:
Never leave your baby unattended while they are eating.
Some preterm babies might appear to have digestion⍰ problems, making faces or being noisy during meals. As long as their poo is soft, there is usually no need to worry. If you are worried about constipation, loose stools, or any other bowel issues during weaning, talk to your healthcare provider.
Cow’s milk as a drink is not recommended for babies under one year old, but you can use it in cooking and cow’s milk-based foods such as cheese and yoghurt. For preterm babies, if they are eating a varied diet, you can start using cow’s milk as a drink when they reach their corrected age of one year. However, if they are not yet eating a variety of solid foods, it is better to continue using formula⍰ rather than cow’s milk to ensure adequate vitamin and mineral intake. Additionally, it is important to start giving your baby drinks from a cup and stop using bottles by 12-18 months old, corrected age for preterm babies.
Some babies born preterm may experience reflux issues due to gastroesophageal reflux disease (GERD) up to age 5, or even later in some cases. GERD is a disease when milk or food flows back up from the stomach into the food pipe (esophagus). It can cause significant discomfort, leading to intense crying, irritability, trouble sleeping, frequent spit-up and even failure to grow. This may affect the baby’s well-being and can also be very stressful for parents. Often, the best approach is to try dietary changes, like giving smaller, more frequent feeds. Usually, symptoms settle slowly over time. If symptoms continue or growth issues persist, seeing a specialist is recommended.
Preterm babies are not more likely to have food allergies than full-term babies. However, if the parents have a history of allergies, their baby may have a higher risk. Avoid removing foods from your baby’s diet without advice, as they could miss important nutrients. If you notice signs that your baby might have a food allergy, you can ask for a referral to a dietitian⍰ or allergy specialist from your family doctor or pediatrician⍰.
Signs of a food allergy can include one or more of the following:
In very rare cases, a food can cause a severe allergic reaction which is life-threatening. If this happens, call your emergency line and get medical help immediately.
Feeding issues are common for many families, and in serious cases, this is known as pediatric feeding disorder. Signs of a feeding disorder include difficulty chewing or swallowing (like choking, gagging, or refusing food), poor weight gain, reliance on supplements or feeding tubes, extreme pickiness, mealtime tantrums, and refusal to use age-appropriate utensils. As children get older, they may avoid social situations involving food, which can impact their social life and relationships. Feeding disorders are more likely in children with developmental or medical challenges, such as autism⍰ or cerebral palsy⍰, and often increase family stress, especially during meals. If you notice feeding-related difficulties, seek early support from your medical team and referral to a speech and language therapist⍰ who specializes in infant feeding.