Feeding your baby can be a powerful way to be close and form a strong connection. It not only boosts your confidence but also allows you to actively participate in your baby's care, creating a strong sense of involvement and connection.
In the neonatal unit, it is crucial for the staff to guide you on feeding your preterm or sick baby, ensuring they receive the essential nutrition they need. Breastfeeding brings many benefits to your baby, especially for premature babies. Beyond the health benefits of breast milk, it provides valuable skin-to-skin contact, helping you and your baby to strengthen your connection.
The let-down reflex
Each time you breastfeed, you might feel tingling or prickling in your breasts, or a sensation like milk is rushing in. This is called the let-down reflex or milk ejection reflex. It is when your body releases a hormone called oxytocin to help with milk flow. Initially, it may take a few minutes for this reflex to kick in, but later it happens within seconds.
The let-down reflex varies among women; some feel a slight discomfort, while others feel nothing at all. Certain actions, such as warm baths, breast massage, or being close to your baby, can trigger this reflex. Staying relaxed and having skin-to-skin contact with your baby can also help stimulate it.
Starting breastfeeding
You may feel unsure about how to begin breastfeeding, especially if your baby has been tube-fed. A nurse, midwife⍰, or feeding specialist at the neonatal unit can guide you through the process. Both parents and other supportive individuals, like grandparents, can play a role in breastfeeding.
Recognizing hunger cues in your baby before breastfeeding is important. Early signs may include putting fingers in their mouth, rooting, or becoming restless.
Breastfeeding positions
Healthcare professionals on the neonatal unit will assist you in finding comfortable breastfeeding positions. They may recommend pillows for support, especially if you have had surgery or your baby was born preterm or sick. Twins or multiples may require extra pillow support for both comfort and baby support.
Challenges with breastfeeding
Breastfeeding challenges can be common among newborns, influenced by factors like age, maturity, and medical conditions. Preterm or sick babies may take longer to develop the skills for breastfeeding. Common challenges include sleepy babies and difficulty finding the right feeding position. Confidence in breastfeeding can take time to develop.
If you are breastfeeding, remember that seeking support can help you navigate these challenges. It is also important to recognize that fathers and supporters can experience challenges during this process, whether they are providing encouragement or looking for ways to assist.
Where to find support
Neonatal units often have feeding specialists, speech and language therapists⍰, specially trained neonatal nurses⍰, or lactation consultants⍰ available for assistance. At home, health visitors⍰, community neonatal nurses, community health workers and general practitioners (GP)⍰ can offer you support and guidance. Do not hesitate to seek help or join breastfeeding support groups in your area for additional assistance and information.
Expressing milk for your baby
Even if your baby cannot breastfeed directly, you can still provide breast milk by expressing. In addition, if breast milk alone does not meet your baby's nutritional needs, your baby's doctor may prescribe a fortifier⍰ to supplement breast milk and help with growth and bone development.
Expressing milk, or collecting breast milk to store for later, is a skill that can take time to learn. In neonatal care, it is important to know how to express milk and care for yourself during this process.
Why express milk?
Expressing milk can be helpful if:
Hospital staff will assist you in expressing milk as soon as possible after birth. This ensures your baby gets the benefits of mother’s own milk even if they are fed via a tube initially.
Starting to express: In the first few hours and days, you will produce colostrum, a thick, yellow milk that is vital for boosting your baby’s immune system and supporting growth. It is normal to express very small amounts initially, but this will increase with time as your breast milk supply becomes established.
Expressing tips
Storing expressed milk
Feeding and growth: Often, preterm or sick babies need additional nutrients. If so, doctors might add a preterm fortifier⍰ to your breast milk.
When to express: Start expressing within two hours after birth and aim for eight to ten times in 24 hours, including at least once at night. Your milk production works on a supply and demand basis, so frequent expressing helps maintain your supply.
Some mothers start to express before their baby is born. Talk to your healthcare provider if you plan to start expressing before your baby is born, as there is a possibility of preterm labor.
The let-down reflex: When expressing, you might feel tingling or a rush in your breasts, known as the let-down reflex, which is triggered by oxytocin. Relaxing, having skin-to-skin contact, or being close to your baby can help trigger this reflex.
Breast massage: Gentle breast massage before expressing can stimulate milk flow. Use warm hands to stroke, knead, and tap your breasts for a few minutes before expressing.
Looking after yourself: Feeding a baby, especially a preterm baby, can be emotionally challenging. If you are feeling overwhelmed, stressed, anxious, or low, do not hesitate to seek support from healthcare professionals or loved ones. There are resources available to help you through this.
Dealing with pressure: Remember, any amount of expressed milk you can provide – even a few drops – benefits your baby. Focus on your progress and avoid comparing yourself to others. Hospital staff are there to support you.
If you cannot express milk right after delivery, please take your time and keep pumping, even if you have only a few drops. It may feel disappointing, but it is perfectly normal for some women to take a little longer to start expressing milk. Stimulating your breasts in the beginning helps signal your body to start producing milk, even if the amount is small at first. A relaxed environment, rest, drinking more fluids, warm breast massages and regular pumping can help you express more milk.
If you cannot always express at the cot side, it can help to have a photo or item that smells of your baby nearby. This can help you to relax and aid milk flow. Partners, family and friends can help by preparing equipment or providing encouragement.
For more guidance on expressing, storing, and defrosting breast milk, speak to the neonatal unit staff. They are there to support you every step of the way.
What if I cannot breastfeed my baby? Alternative ways of feeding
Some babies may not be ready to breastfeed immediately after birth for a variety of reasons. Preterm or sick babies may not be mature or strong enough to breastfeed. It might also be your choice not to breastfeed. There is more than one way to feed your baby:
If you are unable or choose not to breastfeed, it is still possible for your baby to benefit from your breastmilk through expressing. Breastmilk provides important nutrients and protective factors that support your baby’s growth, development, and overall health. If breastfeeding or expressing is not an option, healthcare professionals can guide you through safe and suitable alternative feeding options. You can talk about your worries and feelings. Your midwife⍰, doctors, neonatal nurse⍰ or health visitor⍰ can help.
Your healthcare team might have talked to you about parenteral nutrition or tube feeding. If you are looking for more information, please click here.
Some parents bottle-feed their preterm or sick baby with expressed mother’s own milk, donor human milk or formula⍰.
Recognizing feeding cues for bottle feeding
Just like breastfeeding, it is important to watch for feeding cues when establishing bottle feeding. Early feeding cues include putting fingers in their mouth, making sucking motions, and becoming restless.
Bottle feeding
Your baby will want to be close to you during bottle feeding and you can use this time for skin-to-skin contact. Whenever possible, you or your partner should give the bottle feeds to help your baby learn with you. To ensure you are comfortable and confident, talk to your NICU care team about how to best feed your baby. They will guide you through techniques and recommend positions suited to your baby’s needs.
Here are some helpful questions to ask:
If the milk flows too quickly, it can be hard for your baby to coordinate sucking, swallowing, and breathing. A nurse, speech and language therapist or feeding specialist can advise on teats, bottles, and positions to help with this.
Addressing feeding issues
Some babies may experience low oxygen levels (desaturations) or a slow heart rate (bradycardia) when starting to breastfeed or bottle feed. This can be normal and usually improves over time but may indicate that your baby is not quite ready for oral feeding yet. If you notice these issues, it is important to talk to your NICU care team.
Here are some helpful questions to ask:
Open communication can ensure your baby receives the care they need.
Low oxygen and heart rate during feeding may indicate reflux, where partly digested milk comes back up from the stomach. Reflux is common in all babies but more so in those born preterm or sick and will settle over time as your baby matures.
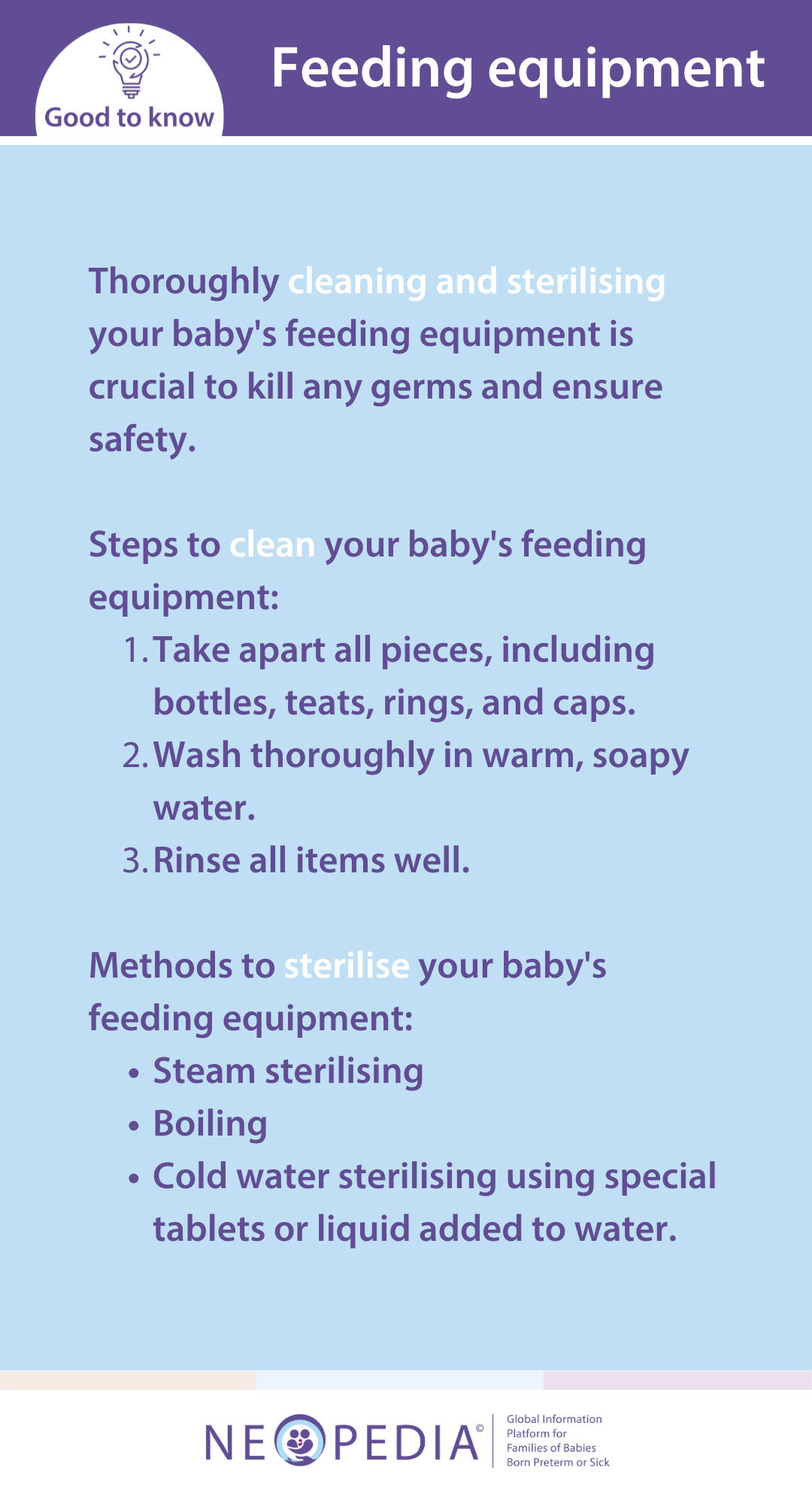
Support and resources
Neonatal unit staff will help you learn how to prepare feeds and clean and sterilize bottles. They may also encourage you to bring bottles and teats from home for your baby to get used to.
Some babies are breastfed and bottle fed, known as mixed or combination feeding. However, it is advisable for your baby to establish breastfeeding before introducing other feeding methods if you plan to mix feed. Talk to your neonatal team, feeding specialist, midwife⍰, health visitor⍰ or general practitioner (GP)⍰ if you are considering mixed or combined feeding.
In certain situations, the neonatal unit staff may suggest that you give your baby a cup of breast milk, particularly if he or she shows signs of wanting to feed but cannot latch on to the breast, or if there is a separation between mother and baby. If you are unsure, ask the staff in the neonatal unit for advice.
Breastfeeding or expressing milk may lead to challenges like:
Sore or cracked nipples can occur when a baby is not well-positioned, causing discomfort and irritation. Blocked milk ducts can cause painful lumps and may develop when the breast is not fully emptied during feeding or expressing.
If left untreated, blocked ducts can lead to mastitis, a breast infection that causes redness, swelling, pain, and flu⍰-like symptoms. If you experience any of these symptoms, speak to a healthcare professional who can guide you toward relief and support.

If feeding your baby is affecting your well-being, it can be helpful to talk to someone. There are many places you can go to feel reassured and supported:
You can contact them for the breastfeeding support you need, or just to listen.
Babies born preterm or sick may need special types of nutrition to meet their unique needs. While many receive their mother’s own milk, some require added nutrients or breast milk fortifiers⍰ to support growth. Donor human milk may also be an option if the mother’s supply is limited. Feeding in neonatal care may differ from what you expected, which can feel unsettling, especially since parents often have less time to prepare. Discuss any concerns or worries with your nurse, midwife⍰ or infant feeding specialist.
Colostrum, the first milk mothers produce, is thick and yellowish, containing proteins and antibodies⍰ that help protect against infections. It is made in small amounts at first, but increases as you express more. Giving colostrum early to preterm or sick babies may improve their feeding and lower their risk of infections.
Breast milk provides ideal nutrition for babies, it supports growth, offers immune protection, enhances brain development, and reduces the risk and severity of conditions like necrotizing enterocolitis (NEC)⍰. If your baby is not ready to breastfeed, hospital staff can help you express milk by hand or with a pump.
Expressed milk can be stored until needed or fed to your baby through a tube until they are ready to breast feed. Neonatal staff can offer guidance as you learn to express milk, and you are encouraged to ask for support if needed.
In cases where mother’s milk is temporarily limited, hospitals may offer donor human milk, especially for babies at high risk for necrotizing enterocolitis (NEC)⍰. Donor human milk can be a valuable alternative to mother’s own milk. Talk with unit staff if you have questions about donor milk or need advice on milk supply.
Preterm or sick babies often require extra protein, vitamins and minerals to meet their high nutrient requirement. A multi-nutrient breast milk fortifier⍰ might be added to their milk to meet these nutrient requirements for enhanced growth and development. If additional milk is needed, doctors may suggest donor milk.
Your baby may be prescribed a special preterm formula, which can be given alongside mother’s own breast milk. Preterm formula has been developed to meet the specific nutritional needs of babies born early. Although it does not contain any of the protective benefits as breast milk, it may be a choice for some babies for other reasons.
Your NICU care team will discuss the use of formula milks with you if it is necessary for your baby. Staff will guide you on safe formula preparation before leaving the unit and local support groups may provide you with further information.