Please consider reading the information that is relevant to you and your little one(s). By doing so, you can avoid overwhelming yourself with too much information in an already distressing time.

Apnea is a quite common concern among babies born preterm, as their delicate nervous system, responsible for breathing, is still developing. After birth, their breathing needs to settle into a regular rhythm. About 70% of babies born before 34 weeks of gestation⍰ may experience apnea to some extent. The earlier a baby arrives, the higher the likelihood of encountering this challenge.
Babies before birth have irregular breathing patterns with frequent pauses, known as periodic breathing. This condition is called apnea, if these pauses last longer than 20 seconds, or if they are accompanied by changes in heart rate or oxygen levels. Fortunately, as preterm babies grow and develop, their breathing tends to regulate, and most outgrow apnea before their expected date of birth.
While most of the time apnea stems from periodic breathing, factors like lung issues or infections can complicate the situation. However, your neonatal or healthcare professional team is keeping a close eye on your baby, monitoring their breathing, heart rate, and oxygen levels. Should apnea happen, they are quick to respond. Sometimes, a gentle touch on your baby's back or feet is all it takes to help them continue regular breathing. Sometimes, the medical team may recommend medication, typically a form of caffeine, to reduce apneic episodes. In more severe cases, oxygen or respiratory support might be necessary.
Asphyxia happens when oxygen supply to the baby, or part of their body, drops to critical levels. This results from either low oxygen levels (hypoxia) or interrupted blood supply (ischaemia). Persistent asphyxia can cause hypoxic ischemia encephalopathy (HIE) and harm vital organs before, during, or after birth.
While in the womb⍰, your baby relies on oxygen from your blood via the placenta and umbilical cord⍰. Asphyxia can occur if this oxygen flow is disrupted, such as when the umbilical cord is blocked or stretched, maternal blood pressure⍰ drops, or the placenta separates prematurely (placental abruption). These complications can be challenging to detect early, however, monitoring the fetal heart rate helps detect asphyxia. Blood tests can also reveal excess acid in the blood, indicating potential issues requiring early delivery.
After birth, prolonged disturbances in breathing or circulation due to severe illness, like infection, can lead to similar events. After delivery, careful examination for signs of altered brain function is important. Tests like electroencephalogram (EEG)⍰ or ultrasound⍰ help assess brain activity and identify any major problems. Later, a magnetic resonance imaging (MRI) may be recommended for further evaluation.
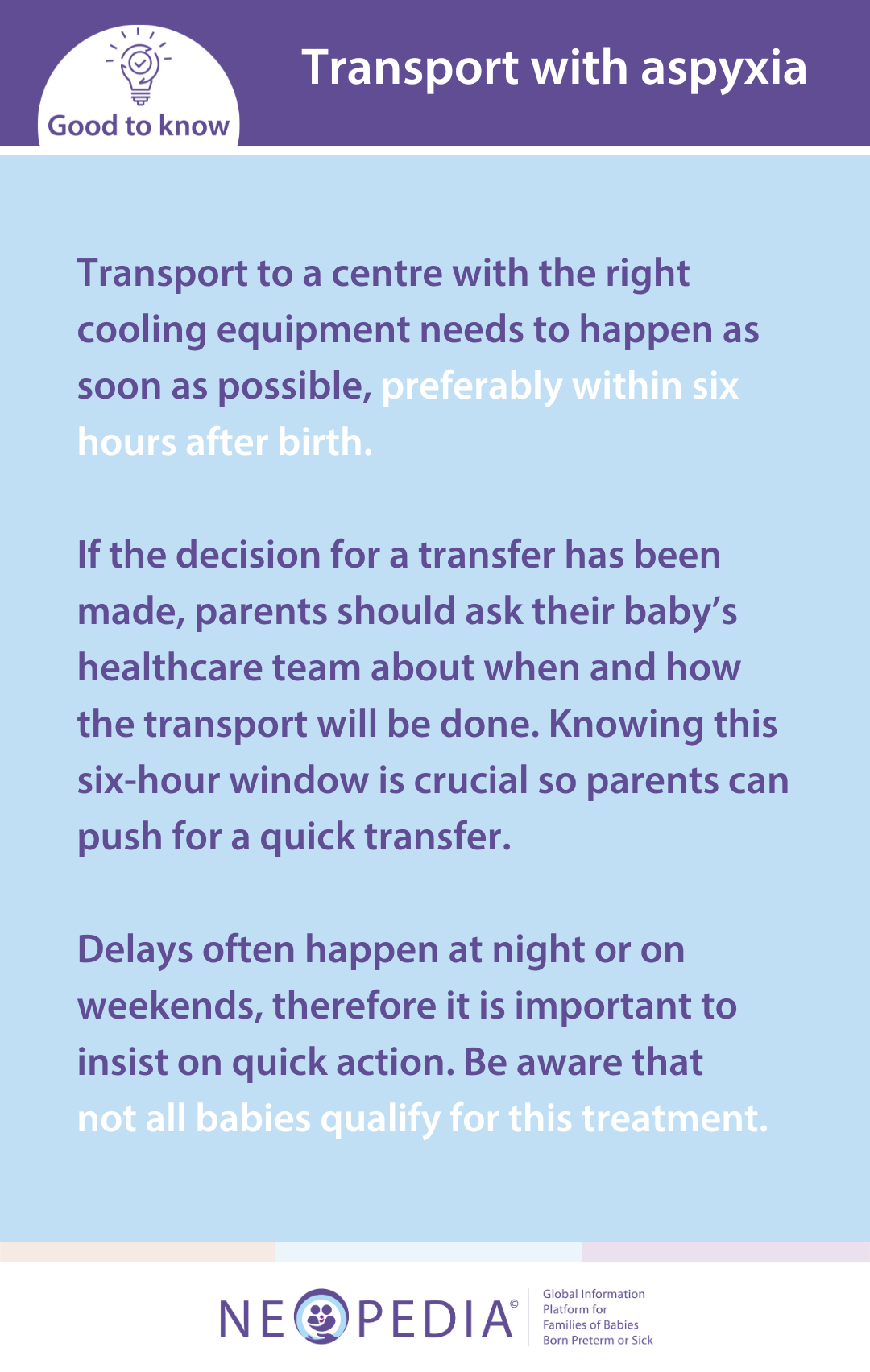
Treatment focuses on making sure oxygen reaches all tissues by increasing oxygen intake or maintaining blood pressure. Sometimes, additional medications are necessary. For babies born after 35 weeks and have a very severe asphyxia, cooling their body temperature to 33-34 degrees Celsius (normal is 37 degrees) may prevent ongoing brain injury. If the baby fulfils the criteria for this treatment and if there are no factors arguing against it (e.g. preterm birth before 35 weeks), this may require transfer to a specialist center.

Bronchopulmonary dysplasia (BPD), also known as chronic lung disease (CLD), refers to persistent lung issues that often affect very or extremely preterm babies (born less than at 32 weeks) receiving oxygen and mechanical ventilation⍰.
Preterm birth may slow down lung development and damage delicate air sacs (alveoli) responsible for oxygen exchange and carbon dioxide removal. BPD manifests with symptoms like rapid breathing, increased heart rate, and low oxygen levels, typically treated with supplemental oxygen.
The causes of BPD are complex and varied. Preterm birth and necessary treatments like oxygen and ventilation can worsen lung damage, especially when coupled with infection. BPD often follows respiratory distress syndrome (RDS)⍰. Typically, if a baby still needs oxygen or respiratory support after a month, BPD is considered. However, most cases improve over time.
Babies needing oxygen at the equivalent of 36 weeks gestation⍰ (around 4 weeks before the expected date of birth or 8 weeks old for a baby born at 28 weeks) are classified as having moderate or severe BPD based on oxygen needs. These categories help decide how long treatment should be and what symptoms might happen later. Monitoring oxygen and blood gas⍰ levels is crucial for managing BPD, with occasional additional respiratory support as needed. Nutritional support is also important for recovery after BPD.
A pneumothorax occurs when tiny lung air sacs (alveoli) become overinflated and burst, allowing air to escape into the space between the lung and chest wall, leading to a potential collapse of the lung. Babies with existing lung conditions like respiratory distress syndrome (RDS)⍰ or pneumonia⍰, those on mechanical ventilators⍰, preterm babies with underdeveloped lungs, and babies who inhale meconium⍰ and amniotic fluid⍰ are most susceptible to pneumothorax. It affects about 1 in 20 babies weighing less than 1500 grams at birth.
Medical professionals may notice signs like a sudden drop in blood oxygen levels or changes in blood pressure⍰ or heart rate. Sometimes, pneumothorax can be identified by shining a light through the baby's chest tissue. Typically, chest X-rays⍰ confirm the diagnosis.
Treatment depends on the size of the rupture. Small ruptures may close on their own or be relieved with a needle. Often, a chest drain is inserted to continuously remove air until the pneumothorax resolves. Oxygen supplementation and gentle ventilation may be necessary, with the potential use of high-frequency oscillatory ventilation (HFOV)⍰ and antibiotics⍰ to prevent lung infections.
In the womb⍰, the blood pressure⍰ in the arteries supplying the lungs and the body is similar. After birth, changes occur and the pressure in the lung circuit decreases, and throughout life it operates at lower pressure compared to the rest of the body's circulation. The pulmonary artery carries blood from the heart's right side to the lungs. Sometimes, this pressure remains high, leading to pulmonary hypertension⍰. This condition can cause various health issues, depending on whether it is sudden (acute) or persistent (chronic).
Pulmonary hypertension is rare in babies, affecting around 1-2 out of 1000 newborns, often during intensive care. It may accompany conditions like asphyxia or BPD. It can happen during acute illness, like those being treated with mechanical ventilation⍰, or persist due to severe lung disease or a patent ductus arteriosus (PDA)⍰.
A telltale sign is the need for high oxygen levels beyond what is expected with lung disease. Diagnosis typically involves ultrasound⍰ (echocardiography). Treatment may involve improved ventilation, like high-frequency oscillatory ventilation (HFOV)⍰, or inhaled nitric oxide gas⍰.
RDS mainly affects babies born too early because their lungs are not fully developed. The risk is highest for those born at the earliest stages: about half of babies born at 26-28 weeks and one-third of those born at 30-31 weeks are affected. Giving steroids to mothers before delivery can help lower the risk and severity of RDS.
Babies start producing surfactant, a substance that helps their lungs stay open, around 23–25 weeks of pregnancy, but they may not have enough surfactant until a few days after birth. When babies have trouble opening their lungs or surfactant is inactivated because of problems like asphyxia or infections, symptoms of RDS may appear as well.
To treat RDS – and in some cases to help prevent it – replacement surfactant can be given directly into the baby’s lungs soon after birth. Blood tests and chest X-rays⍰ are used to diagnose RDS and check how well the treatment is working. Along with this treatment, babies may need extra help with breathing, such as oxygen, CPAP, medications, or mechanical ventilation⍰. Most preterm babies recover from RDS without major issues within the first week.