Most parents feel uncertain about how to support their baby in the neonatal unit initially. Taking an active role can bring positive changes for you, your baby, and your family. While it is okay to feel a bit unsure at the start, many families discover that getting involved is a process that builds confidence over time.
What is IFCDC/FCC?
IFCDC stands for infant- and family-centered developmental care, also known as family-centered care (FCC) or family integrated care in some countries. This approach supports your baby's development through more than just medical care and ensures that you and your baby are the center of care.
It includes managing what your baby sees and feels, using techniques like specific holding and positioning, practicing skin-to-skin care, and actively involving parents in decisions about their baby’s care and treatment. Different countries may use slightly different terms, but the goal is always to support both the baby’s growth and the family’s role in their care.

How to create a supportive environment
Creating a nurturing environment for your baby's growth is a shared effort between the NICU care team and parents.
Using soft nests, comfortable positions, and carefully managing noise and light around your baby can help create a calm, soothing space. The NICU care team also work to align medical care with your baby’s natural sleep-wake cycles and to minimize pain whenever possible.
The goal of Infant- and Family-Centered Developmental Care (IFCDC) is for parents and the NICU care team to work together, providing an environment that supports your baby's healthy growth and development.
Preterm babies may encounter health challenges after they are born. Some may also experience delays in growth and development, especially those who are very preterm or have medical complications.
Your baby's development will be assessed regularly by healthcare professionals to make sure they are progressing well and to address any concerns.
Some babies may need extra support from a physiotherapist⍰ or occupational therapist⍰ to develop strength and muscle tension, get help with feeding problems and sensory problems. These therapists can show you gentle exercises or activities that you can help with at home.
If you have any concerns about your baby's development, discuss them with your NICU care team.
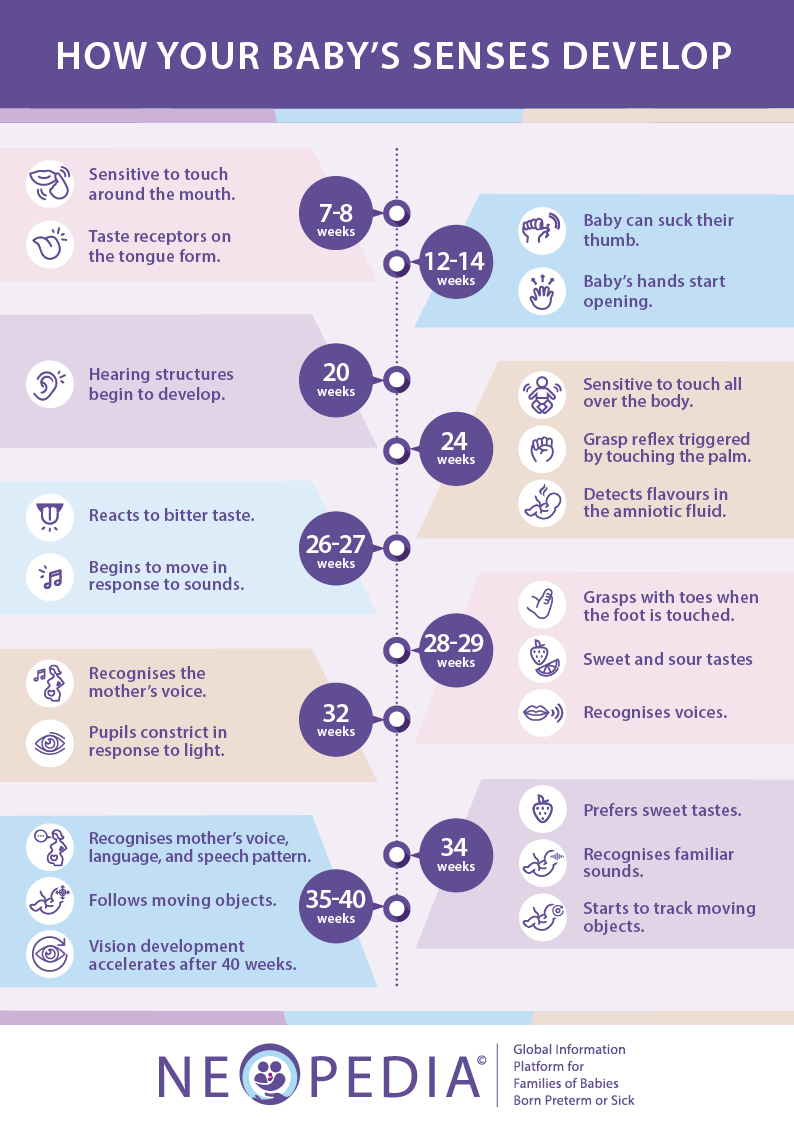
Around 7-8 weeks:
Around 12-14 weeks:
Around 20 weeks:
Around 24 weeks:
Around 26-27 weeks:
Around 28-29 weeks:
Around 32 weeks:
Around 34 weeks:
Around 35-40 weeks:
Signs that your baby is comfortable can include:
If your baby shows any of the signs below, they may be uncomfortable. You or someone from the NICU care team should make adjustments to help them feel more at ease. This could involve changing their diaper (nappy), ensuring they are positioned comfortably, feeding them, or adjusting the temperature, noise, or light around them. If you are unsure about their comfort or have any concerns, do not hesitate to speak with a healthcare professional for further support.
For babies, adjusting to changes in temperature is not as easy as it is for adults. Babies born preterm often have very little body fat. When a baby's body temperature is too low, they use more energy and oxygen to stay warm.
It is important to keep your baby’s surroundings at the right temperature and ensure their skin stays dry and warm. After birth or a bath, using warm blankets and having skin-to-skin contact with a parent can help warm and dry your baby quickly. If you are unsure about keeping your baby warm, ask a healthcare professional for guidance.
Just like adults and older children, babies feel pain, and it is important to make sure they feel as little discomfort as possible.
Babies, especially those born early or sick, need extra care when they undergo medical procedures, like having blood taken or having surgery. Doctors and nurses have studied the signs of pain in babies and may use a checklist to track these. They can teach you how to look for the signs of pain your baby might show. If your baby seems stressed, there are many things healthcare professionals can do to help. This is especially true when preparing for certain procedures and they know that pain will occur.
They might change the environment by making it quieter and dimming the lights. They can also let your baby be close to you, engage in skin-to-skin care and breastfeeding, providing glucose (a form of sugar) to the baby, or let them suck on a pacifier⍰. Parents being there can really help and support the baby during and after a painful procedure. With the help of the NICU care team, parents can become experts in their baby’s behavior and manage their pain and stress by comforting them and changing the environment. If your baby needs extra help, the NICU care team might give them pain-reducing drugs (analgesics) to make them feel better.
All these things are done to make sure your baby in the neonatal unit is as comfortable and content as possible, even when they need procedures.
Understanding your preterm baby’s muscle tension and positioning is an important part of their care. Because their muscles are still developing, preterm babies tend to have lower muscle tension than full-term babies. Gently helping them find comfortable positions supports the healthy growth of their muscles and bones.
Creating a "nest" using rolled-up sheets or blankets shaped into a wide, thick band around your baby can provide comfort. This setup gives your baby boundaries to touch, much like the womb⍰, which helps them feel secure and keeps their arms and legs in a supportive position – important for future milestones like crawling, standing, and walking. As much as the babies like nesting, this should only be used under adult supervision.
Good positioning can also reduce your baby's stress, improve their breathing and digestion⍰, and support healthy blood flow. If you have questions, do not hesitate to ask your NICU care team for guidance.
Different lying positions for your baby:
Lying on the tummy (prone position)
Lying on the back (supine position)
Lying on one side (lateral position)
Babies have two main sleep states: deep or quiet sleep and active or light sleep, also known as rapid eye movement (REM). Additionally, they go through different behavioral states, ranging from drowsiness to being actively awake and fussy to crying.
It might be a bit tricky to know exactly what state your baby is in, but recognizing these behavioral states can help you understand when your baby is ready for interaction and when it is time to help them get some rest.
Deep/Quiet sleep:
Light/Active sleep:
Drowsy:
Quietly awake:
Actively awake:
Crying:
Several factors affect your baby's sleep in the neonatal unit, such as timing care around their alertness, adjusting noise and light for a calm environment, ensuring comfortable positioning, and feeding based on your baby’s needs.
Parents play a vital role in helping their baby's sleep. They can settle their baby to sleep effectively. Skin-to-skin care and the parents' voice also contribute to promoting sleep. The NICU care team can guide you in supporting your baby for restful sleep.